Tobacco Cessation in Kenya
The majority of people who use tobacco in Kenya would like to quit. 71% of tobacco smokers aged 18 and over planned to quit at some point.
Tobacco users in Kenya do not receive the cessation support they require to successfully stop using tobacco.There are only 34 accredited tobacco use disorder treatment centers across 13 of the 47 counties in Kenya.
More than 70% of the 1.3 billion tobacco smokers globally do not have access to the facilities/resources they need to successfully quit smoking.
Quitting tobacco use is imperative as it improves health, saves lives, and reduces financial burdens. The majority of smokers who try to quit do so without any help, and most of the time they fail to stop smoking. Cessation has a greater chance of success if a combination of medication, counseling, and other remedial programs is provided to tobacco smokers. For example, one study reveals that only 5% of those who try to quit tobacco smoking on their own without any help succeed, compared to 20% of those who receive cessation support.This page provides information on the reasons Kenyans start using tobacco, the levels of public awareness of the harms of tobacco use, the percentage of smokers willing to quit and the reasons why they intend to quit, the availability of pharmacotherapies and treatment facilities for tobacco use dependence, and the benefits of quitting.
Any level of tobacco use is harmful to health. The desire for nicotine is the main driver behind tobacco usage.
With prolonged use of tobacco, physical dependence develops due to an increase in the number of nicotinic cholinergic receptors in the brain. Initial experimental or occasional tobacco use can easily progress to what doctors call “tobacco use disorder”. Doctors diagnose tobacco use dependence when the individual exhibits any two of the following characteristics over a 12 month period:Symptoms of Tobacco Use Disorder
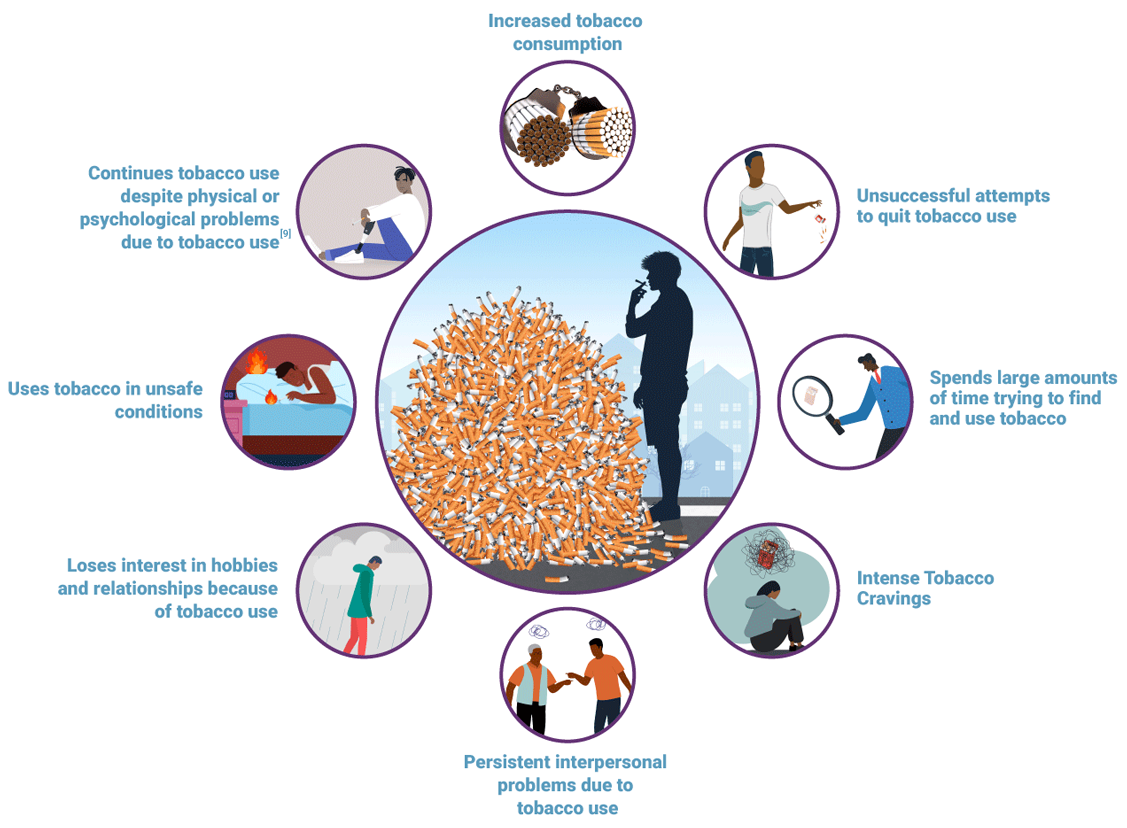
Ref 9
Due to the effects of nicotine, tobacco use disorder sufferers may experience nausea, decreased appetite, weight loss, sleeping problems, low blood oxygen levels, emphysema, high blood pressure, anxiety, and irritability. Nicotine withdrawal symptoms include headaches, flu-like symptoms, difficulty concentrating, and depression.
Risk Factors for Tobacco Use Dependence
Across the world, tobacco use is more common among people of low socio-economic status, people with mental disorders (such as attention deficit hyperactivity disorder, schizophrenia, and personality disorders), and people with other substance use disorders. In Kenya, tobacco use is more common among groups of people with no education (23.2%) and least common among those who have achieved the highest level of education (6.7%).
Other risk factors for tobacco use in Kenya include being male, living in urban areas, and having friends who use tobacco. In addition, people who suffer from mental disorders have a higher chance of using tobacco. They smoke two to four times as frequently as the overall smoking population. As such, they have a higher dependence on nicotine, stronger withdrawal symptoms, and lower cessation rates.Reasons for Tobacco Use
The majority of Kenyan smokers began consuming tobacco when they were teenagers, with peer pressure being the primary factor behind their original cigarette usage.
Individuals who have smoking friends and/or parents are more likely to begin smoking than those who do not.Aside from peer pressure, the following are other key reasons that make individuals take up smoking (as highlighted by studies in Kenya):
use of alcohol and drugs, access to cigarettes in a social setting, and stress factors.In fact, more than 50% of the respondents to a qualitative tobacco study in Kenya indicated that peer pressure was the primary driver behind cigarette usage.To me, myself, I would like to quit but in the society, see, in the society where I live, most of my friends are smokers. I have seen some of my friends who had quit cigarettes for maybe two years, one year, three months, but when they come back to us, they find themselves back to….to cigarettes.
(42 year old male, Urban, Current tobacco user)
The adoption and enforcement of bans on tobacco advertising, promotion, and sponsorship (TAPS) in Kenya has reduced the influence of TAPS as a driver for tobacco use. According to one International Tobacco Control (ITC) survey, only 8% of tobacco users and non-users in Kenya noticed adverts designed to promote tobacco consumption.
Majority of the public know of the dangers associated with tobacco smoking.
Percentage of Tobacco Users Vs Non-Users Who Believe that Smoking Causes Various Health Effects, 2018
More non-tobacco users than tobacco users believe that tobacco use leads to several serious illnesses. Approximately 94% of non-tobacco users believe that tobacco use leads to lung cancer, while 84% of tobacco users believe the same. Other illnesses cited by both tobacco users and non-tobacco users include throat cancer, chronic obstructive pulmonary disease, mouth cancer, heart disease, stroke, tuberculosis and impotence.
Knowledge of the harms of tobacco use is not only restricted to adults. Seventy five percent of youths aged 13-15 interviewed in the 2013 Global Youth Tobacco Survey also indicated that other people’s tobacco smoking was harmful to their health. In a more recent study by the National Authority for the Campaign Against Alcohol and Drug Abuse (NACADA), 91% of class 5-8 pupils surveyed considered tobacco to be harmful.Percentage of Smokers Who Plan to Quit in the Future
The majority of tobacco smokers in Kenya would like to quit. 77% of current tobacco smokers aged 15 and over planned to quit in 2014. According to the ITC survey, 71% of smokers aged 18 and over planned to quit in 2018.
Quit intentions in Kenya are higher than the global average – across countries where the Global Adult Tobacco Survey has been carried out, over 60% of smokers indicated that they intend to quit, and over 40% had attempted to quit in the 12 months preceding the survey.
52% of tobacco smokers aged 15 and over had attempted to quit smoking in the previous 12 months.
According to the ITC survey, only 39% of smokers aged 18 and over had attempted quitting in the past, while 61% had planned to quit. Furthermore, only half (50%) of smokeless tobacco users had planned to quit in future. Notably, over half of the tobacco smokers across Kenya’s provinces planned to stop smoking, except smokers in North Eastern (24%) and Nairobi (39%). There are no cessation facilities available in the North Eastern region.Percentage of Smokers Who Plan to Quit in the Future, 2018
The ITC survey also assessed whether respondents had sought the services of health providers for any reason in the preceding six months and gauged whether they received various types of support for smoking cessation during any visit.
Only 37% of tobacco users who visited a health professional in the previous six months received advice to quit. The ITC findings were similar to those of the GATS, which highlighted that 34% of smokers that had visited a health professional received advice about tobacco cessation.The ITC survey also found that only 4% of tobacco users received advice or information about quitting from telephone or quitline services in the preceding six months.
These results indicate that tobacco users in Kenya do not receive sufficient cessation support to successfully stop using tobacco. Research evidence shows that advice from health professionals can help smokers to quit, and that even brief simple advice can increase cessation rates by 1% to 3%.
To improve cessation rates in Kenya, healthcare providers across the country need to be sensitized on how to offer brief cessation counseling advice to patients.Reasons Motivating Quitting
Health reasons are the primary factors driving the desire to quit smoking.
According to the GATS and ITC surveys, tobacco’s negative health effects were the primary factors driving 75%
of current smokers to quit (65% of former smokers had quit due to these reasons). The need to set an example to children (61% of respondents) and the warnings on cigarette packs (58%) were also highlighted as key motivators. The high cost of tobacco products was also cited as a key reason for quitting by 28% of female smokers compared to 4% of male smokers in the GATS report. Public disapproval about the use of smokeless tobacco products was similarly highlighted as a reason to quit among users of these products.Percentage of Smokers and Smokeless Users Who Highlighted Various Reasons for Quitting, 2018
The introduction of pictorial health warnings in 2014 substantially increased awareness about the dangers of tobacco use and boosted the motivation to quit. In fact, 75% of smokers reported that the new pictorial health warnings made smoking seem more dangerous. Results from the ITC study show that increasing the size of the pictorial health warnings on cigarette packs and implementing pictorial health warnings on smokeless tobacco would further increase the impact of tobacco health warnings in Kenya.
There are various interventions in Kenya to help tobacco users quit
Smoking cessation refers to the process of ending the consumption of tobacco products.
There are different avenues that smokers can use to quit. The Ministry of Health of Kenya has developed the ‘National Guidelines for Tobacco Dependence Treatment and Cessation’ which provide a step-by-step method of helping individuals stop tobacco consumption. The Kenya Tobacco Control Act further advocates for tobacco control education and provision of cessation services.Types of Interventions
Counseling (Behavioral Support)
Counseling (Behavioral Support)
Behavioral and pharmaceutical interventions can be used to help people stop smoking.
Behavioral interventions cover services given to tobacco smokers by health providers, including routine counseling sessions and consultations that provide smokers with advice. Compared to self-help efforts, group therapy sessions are more beneficial in helping people stop smoking. Another study on tobacco cessation behavioral interventions among patients with mental illness in Kenya similarly showed that group therapy sessions are beneficial and aid in cessation. Behavioral therapies are highly successful in aiding cessation when combined with pharmacological interventions.Pharmacotherapies
Phramacotherapies
Pharmacotherapies include nicotine-based and non-nicotine-based medications that are given to the smoker, such as nicotine replacement therapies, bupropion, and varenicline.
In Kenya, available pharmacotherapies include:
- Bupropion (also known as Zyban, Wellbutrin, or Aplenzin) – Bupropion is classified as an antidepressant. It is used for tobacco use disorder because it reduces cravings and nicotine withdrawal symptoms by acting on the chemicals in the brain responsible for nicotine cravings. Bupropion does not contain nicotine and works best if it is consumed one or two weeks before quitting. In Kenya, a prescription is required for Bupropion.
- Varenicline – Varenicline (Chantix) is an oral prescription drug. It acts as a nicotine antagonist and agonist. As an antagonist, it blocks nicotine’s connection to receptors in the brain, making tobacco use less satisfying and desirable. As an agonist, it mimics the effects of nicotine, thereby reducing cravings and withdrawal symptoms. Treatment usually starts 1-2 weeks before the quit date.
- Nicotine Replacement Therapy (NRT) – NRT aims to partially replace the nicotine found in cigarette products while removing hazardous chemicals. Nicotine patches, nicotine gum, nicotine inhalers, nicotine lozenges, and nicotine nasal sprays are various forms of NRT available in Kenya. NRTs lessen nicotine addiction withdrawal symptoms, allowing tobacco users to concentrate on the psychological components of quitting. The best outcomes are obtained when behavioral counseling and follow-up sessions are used at the same time.
In Kenya, Bupropion (150mg tablets), and Nicotine Replacement Therapy (NRT (as polacrilex (/polacrilin complex), chewing gum (2mg and 4 mg), and transdermal patches (7-21mg/24hours) are listed as essential medicines.
NRTs are available from private pharmacies in Kenya without a prescription. The Kenya National Health Insurance Scheme (NHIF) covers these medications following admission to a hospital.Tobacco Cessation Treatment Facilities
Availability of cessation services is uneven across the country
There are 34 substance abuse treatment centers among those accredited by NACADA that have the capacity to provide tobacco cessation interventions. While most are privately owned, a few are managed by non-governmental organizations and the government. Out of the 47 counties in Kenya, only 13 have treatment centers. Of these 13, four counties (Kajiado, Kiambu, Mombasa, and Uasin Gishu) have the greatest numbers of centers. The rest only have one or two facilities available to citizens. NACADA also provides a toll-free number that individuals can use to speak to counselors about alcohol and drug addiction. This service is free of charge on Safaricom and Telkom lines and is available 24 hours a day, every day.
A host of services are available at NACADA-accredited facilities, including psychiatric evaluations, screenings and assessments, community outreach programs, detoxification programs, daily exercise and physical fitness activities, in-house gender-based violence prevention sessions, psycho-educational classes, individual, group, and family counseling sessions, naltrexone implantations, narcotics and alcoholics anonymous meetings, 12-step programs, health talks, and tobacco cessation therapies. These services can be received at the locations indicated on the map.
Cessation Best Practices
In 2018, only 23 countries (sixteen high-income, six middle-income and one low-income) offered comprehensive cessation support for tobacco users seeking help to quit.
Best practices in the provision of cessation services include: brief advice offered at the primary care level, national toll-free tobacco quit lines, partially or fully cost-covered nicotine replacement therapies and cessation interventions integrated into universal health coverage, and the use of digital and mobile technologies to empower those who want to quit.
Examples of best practices around the world are provided below:
India has greatly increased access to cessation services through an innovative program that allows participants to enroll and receive tailored support to quit on their mobile phones.
This innovative program – called QuitNow – was established in 2015. Also referred to as a ‘mCessation’ program, QuitNow’s development was supported by several entities, including WHO, the Indian Ministry of Health and Family Welfare, the Indian Ministry of Communication and Information Technology, and the International Telecommunication Union’s “Be He@lthy, Be Mobile” initiative. 19% of the users of the service self reported that they had abstained in the preceding 30 days in 2015.
Tobacco control measures that are implemented concurrently have significantly better outcomes than corresponding interventions undertaken in isolation.
In Brazil, a national quitline was included in the graphic health warning messages printed on cigarette packages. The coupling of these two measures had a magnified impact on cessation – in fact, the quitline in Brazil received an unprecedented six million calls in the first year (2011), more than all other quitlines globally at that time.
Pakistan, Bangladesh and Nepal have integrated behavioral support services with specialized healthcare programs to expand access to cessation services.
In these countries, behavioral support services have been integrated into tuberculosis (TB) treatment programs. Specifically, health workers received training on providing brief behavioral support, and TB case reports were revised to include the smoking status of the patients. Research on cessation was also embedded into TB treatment programs.
Altogether, this integration had a positive effect on cessation across the three countries. The training builds the confidence of health workers in delivering cessation support to patients, and the changes to reporting forms provided program-level data on tobacco use among TB patients (as well as the cessation support being offered to such patients). When interviewed, the TB patients who used tobacco confirmed that they had received brief advice to quit.
Moreover, training materials were disseminated beyond the national TB healthcare sites across the three countries, indicating that there was a horizontal scaling up of cessation efforts.
Thailand earmarked revenue from tobacco taxes for cessation.
In Thailand, revenues from tobacco and alcohol excise taxes have been directed into the Thai Health Promotion Fund since 2009. The Thai Health Promotion Fund uses these revenues to financially support the National Tobacco Quitline as well as improve cessation services in government hospitals. The Ministry of Health has used this financial support to treat up to 22,000 smokers a year with a smoking cessation rate of 33%.
Health benefits
Over time, people who quit smoking see many health benefits. After a person smokes their last cigarette, their body begins a series of positive changes that continue for years.
Life Cycle of Recovery
How Quickly Health Improves after Quitting Smoking
Economic Benefits of Quitting
Intro text: Smoking cessation has economic benefits for individuals, their families as well as healthcare systems.
Individuals that stop smoking save money as they no longer need to purchase tobacco. Smoking cessation also reduces healthcare costs at the individual and hospital level, reduces absenteeism at work (arising from tobacco related illnesses), and lowers the costs involved in cleaning up after smokers (e.g., the costs of picking cigarette ends, sweeping ash, and repairing damage to floors and furnishings).
The infographic below compares the amounts an average Kenyan smoker spends on tobacco to the costs of treating tobacco dependence and the economic costs to the healthcare system.

ref1
ref2 ref[43]This section addresses and counters the arguments used by the tobacco industry to promote ineffective tobacco cessation, deter smokers from quitting, and prevent governments from regulating e-cigarette use.

Myth: Novel tobacco products can be used as cessation aids
Fact: E-cigarette use can be a gateway to ordinary cigarette use.

Myth: Effective regulation of novel tobacco products, such as taxation and marketing restrictions, denies smokers access to reduced-risk products that could reduce the public health burden of tobacco use.
Fact: Novel tobacco products are not harmless. The tobacco industry exploits regulatory loopholes to package and market novel tobacco products as consumer products rather than medicines.

Myth: It is nearly impossible to quit tobacco or other nicotine products, no matter how many times or how hard you try.
Fact: Quitting tobacco products is difficult because nicotine is so addictive and people often try to do it on their own without counseling or enough medication. However, it is doable, especially with support.